Aortoenteric fistula usually occurs at the proximal anastomosis (region of infrarenal aorta and 3rd/4th part of the duodenum) and can result in massive bleeding into the bowel. Although AEF is usually separated from "perigraft infection" in terms of classification, the graft is invariably infected in aorto-enteric fistula (backflow from enteric contents). Infection of the graft causing the AEF is also considered a significant etiology (40% of infected grafts become AEFs) as prosthetic material can serve as a nidus for bacterial growth. Some feel that infection may play a role in all AEFs, but many may arise from lower-grade infections.
Graft-enteric fistulas can potentially occur anywhere along the graft, although they tend to occur more proximally. Of course, they're more common at weak points such anastomotic suture lines, but a fistula can occur even with native aneurysms (considered a primary aorto-enteric fistula).
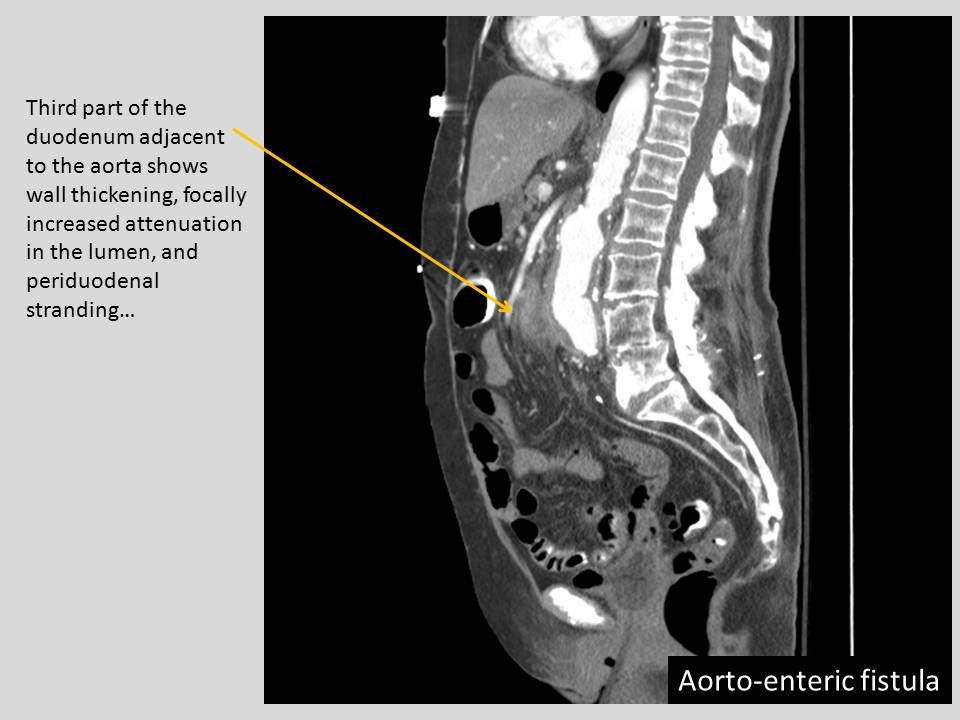
So what are the findings with an aorto-enteric fistula? If upper GI bleeding is the provisional diagnosis and the patient is stable, EGD is often used as a first line modality. But if it's not suspected / or if the EGD is not definitive, then the patient may go to CT. As the name AEF implies, you look for an exchange of contents between the aorta and the bowel. Gas into the area area around the graft, and blood into the adjacent bowel. Actual visualization of extravasation is rare.
Angiography is only rarely employed for diagnosis of an AEF (and it cannot diagnose a GEE (below)). Angiography may be negative or present with a small "nipple" at the anastomosis (most patients with an AEF have a thrombus temporarily occluding the fistula). Frank extravasation is rare.
Fortunately, the occurance of aorto-enteric fistulas is not common (Primary: ~ 0.05%, Secondary ~1%). A "sentinel bleed" can occur before later and more devastating hemorrhage.
The etiology of primary AEF can also arise from the bowel... a penetrating dodenal ulcer or a small bowel neoplasm can move into the nearby aorta. Similarly, diverticulitis or appendicitis can potentially involve an adjacent aorta.
An aortic etiology typically comes from an aneurysm (the continual pulsation is thought to contribute to fistual formation)... but they don't have to exclusively occur from an aneurysm; aortitis can also be a causative factor.
Another entity to mention is Aortoparaprosthetic sinus (a.k.a. "Graft-enteric erosion" GEE), which is basically an AEF without a connection to the aortic lumen. Instead, pulsatile pressure and mechanical erosion of the bowel result in infection of the graft with enteric flora. This process is not as common as AEF.
Although less common that with repair grafts, AEF has been noted to occur after EVAR placement.
Therapy for an AEF? Conservative therapy is not an option for resolution of the AEF. Graft removal (with extra-anatomic bypass) is the best option in a stabilized patient. Placement of stent grafts as a temporizing measure is evolving, it is not considered definitive therapy since it involves placing hardware into an infected field.
---
1. Vascular and Interventional Radiology: The Requisites. Kaufman JA, Lee MJ, et al. 1st ed. 2004
2. Vu QD, Menias CO, Bhalla S, et al. "Aortoenteric Fistulas: CT Features and Potential Mimics" January 2009 RadioGraphics,29, 197-209.
3. "Vascular and Interventional Radiology" Valji K, ed. 2nd ed. (2006).
4. "Rutherford's Vascular Surgery" Cronenwett and Johnston. 7th ed (2010) Chapter 42.
