While we're on the subject of anastomotic vascular
arcs, there's another eponymous and infamous arc in the human body...
the Arc of Riolan. Some claim that Riolan did not clearly identify the artery and prefer the term "meandering mesenteric artery (of Moskowitz)." Some claim that the two are different arteries. Some even claim a third mesenteric anastomotic artery... but for this post we'll assume they're all the AoR.
Whereas the Arc of Buhler connects the celiac and SMA vascular supplies, the Arc of Riolan (AoR) helps connect the SMA and IMA.
The SMA and IMA routinely anastomose through the Marginal Artery of Drummond and the AoR is essentially a shunt bypassing this smaller, more tortuous vessel... shunting
between the proximal middle colic artery of the SMA and the proximal left colic artery of the IMA.
Some studies report the AoR as occuring in 7-10% of the population. CTA or conventional angiogram is the easiest way to identify the artery, which is usually a very large and tortuous artery of uniform caliber in the left upper quadrant of the abdomen. It may not always be easy to see its origin from the middle colic, but usually its connection to the left colic is more clear. Differentiation of the Arc of Riolan from the Marginal artery of Drummond is straightforward in that 1) the Marginal artery of Drummond is never tortuous and runs parallel to the descending colon, and 2) the Marginal artery is rarely visualized on angiogram without vasodilators.
The AoR can be important as an anastomotic channel in the setting of stenosis or occlusion of either the SMA or IMA.... the
direction of flow in the artery helping to differentiate one from the
other.
and it can also be important in the setting of distal abdominal aortic occlusion with anastomoses to the iliac arteries through the superior rectal artery and then to the lower extremities through the external iliac artery. It has been claimed that in total abdominal aortic occlusion, the anastomotic arteries can dilate to 2-3x their normal diameter, and reduce in size after aortic thrombectomy.
 |
| Dilated Arc of Riolan / meandering mesenteric artery due to celiac and SMA stenoses from Takayasu's arteritis. |
...and the AoR can also be a help in the setting of endoleak of aortic stent grafts...
If the IMA is not thrombosed at the time when an EVAR stent graft is placed, the potential for type II endoleak exists, with back-filling of the aneurysm sac through the IMA or lumbar arteries.
 |
| Axial and sagittal CT with contrast demonstrate and enlarging aneurysm sac after stent placement. A small blush of contrast was noted at left anterior aspect of the aneurysm sac (yellow arrow), compatible with a type II endoleak and retrograde filling from the IMA. |
 |
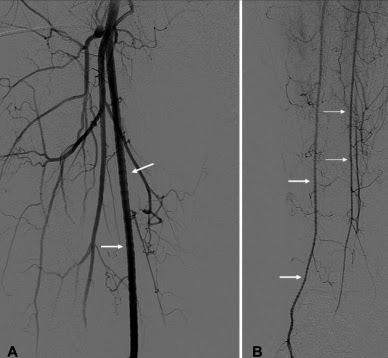
| SMA arteriogram of the same patient shows an Arc of Riolan, indicative of IMA stenosis (although apparently not complete thrombosis). Note that the Marginal Artery of Drummond is not visualized on angiogram. |
 |
| Selective catheterization of the Arc of Riolan. |
One solution for this situation is to occlude the lumbar arteries or IMA at their origin, and the Arc of Riolan can be a handy, relatively large arterial access to the aneurysm sac, allowing glue or coil embolization of either the lumbar arteries, the IMA, or both, depending on the inflow and outflow situation of the type II endoleak.
 |
| Coiling of the origin of the IMA |
---
1. McDermott S, Deipolyi A, Walker T, et al. "Role of preoperative angiography in colon interposition surgery." Diagn Interv Radiol 2012; 18:314–318.
2. Skandalakis Surgical Anatomy: Chapter 12. Great Vessels in the Abdomen. (2004)
3. Fisher Df, Fry WJ. "Collateral Mesenteric Circulation" Surgery, Gyencology and Obstetrics.
1987, 164(5):487-492.
4. Gourley EJ, Gering SA. "The Meandering Mesenteric Artery: A Historic Review and Surgical Implications." Disease of the Colon & Rectum. Vol 48:5 (2005) pp 996-1000.
5. Kasiraja K, Matteson B, Marek JM, Langsfield M. "Technique and results of transfemoral superselective coil embolization of type II lumbar endoleak" Journal of Vascular Surgery. Vol 38:1 (July 2003) pp. 61-66.