The advantages?
- MRA with quick concurrent diffusion-weighted MRI sequences of the brain can evaluate infarction much better than CTA. (Cerebral infarction is documented in 42% of spontaneous carotid dissections)
- T1-weighted images of the neck are superior for evaluation of hematoma than catheter-based angiography (although CTA is also good for this).
- MRA avoids the 1% stroke risk of catheter-based angio (CTA also does this, of course)
- MRA avoids potential contrast-induced nephropathy (assuming that most patients being evaluated for dissection are young, renal failure and the risk of NSF are not as much of an issue)
- MRA avoids ionizing radiation
 |
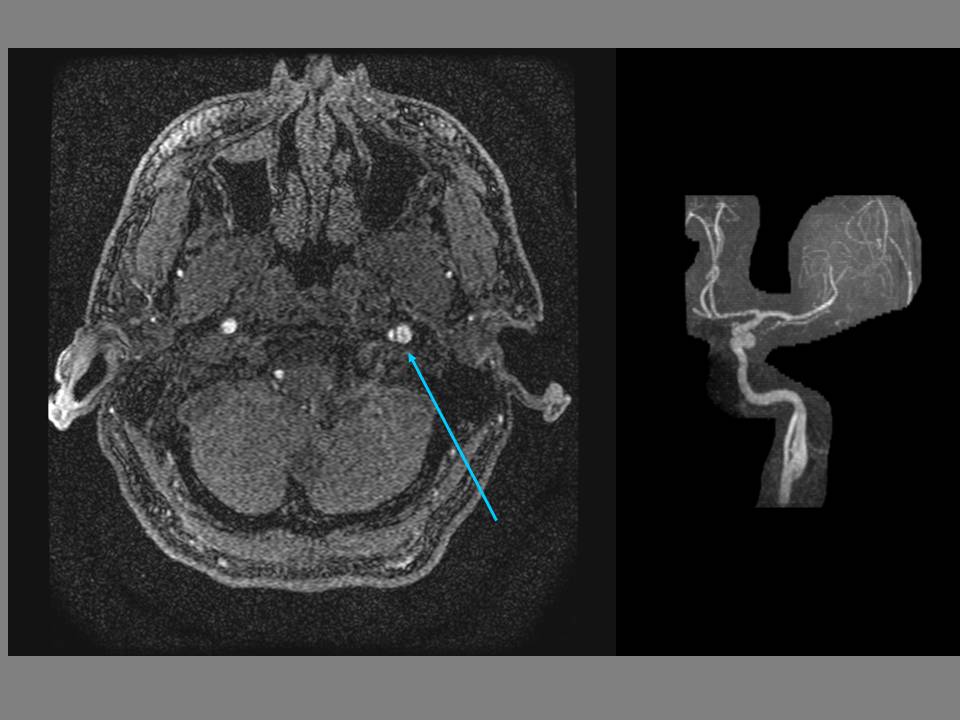
| Left internal carotid dissection with aneurysm (arrow). 3D TOF MIP MRA. |
The disadvantages?
- The spatial resolution of MRA is not quite as high as that of CTA (perhaps Ablavar (10/19/12 post) would change this?), and concomitant evaluation of the vertebral arteries in the setting of trauma is better with CTA.
- Although the false lumen would be identified on the T1-weighted sequences, turbulent flow in an aneurysm can lead to signal drop out and underestimation of the size of the aneurysm on the MRA.
- MRA can be affected by metallic density artifact in then neck, rendering it dangerous or useless (CTA also has the problem of streak artifact with metallic densities). MRA is also affected by neck stablization hardware.
- MRA is slower than the other modalities.
The target population for carotid artery dissection is generally younger, and the lack of ionizing radiation in MRA is attractive, especially since these patients often receive multiple follow-up studies to evaluate the resolution/progression of the dissection and hematoma. Depending on your level of suspicion for acute infarction (in which diffusion-weighted sequences would be invaluable), CTA in the ED with MRA follow-up would seem a reasonable algorithm.
Recent reports claim that a T1 CUBE black blood sequence may offer improvement in detection of dissection compared to conventional axial T1 sequences... no problem, you just need that 3T scanner.
---
1. "Rutherford's Vascular Surgery" Cronenwett and Johnston. 7th ed. (2010)
2. Vertinskya AT, Schwartzb NE, Fischbeinc NJ, et al. "Comparison of Multidetector CT Angiography and MR Imaging of Cervical Artery Dissection" AJNR October 2008 29: 1753-1760
3. Edjlali M, Roca P, Rabrait C, et al. "3D Fast Spin-Echo T1 Black-Blood Imaging for the Diagnosis of Cervical Artery Dissection"